Meet the biophysicist whose seizure-detection company is using AI to get a better read on people’s brains
Nonconvulsive seizures can kill patients in the ICU. In one study, one-third of such patients died. Yet getting a patient diagnosed with a seizure in the ER or ICU is not easy. It requires an electroencephalogram (EEG), which measures electrical activity in the brain. Getting an EEG can take anywhere between a few hours to a couple of days, since there is a shortage of EEG technicians. Post-pandemic, one study reported that EEGs have declined by 50%. If a doctor decides to treat a patient proactively without a diagnosis, treatment can be invasive and might mean being intubated and being dosed with benzodiazepines. Taking benzodiazepines prior to an EEG makes it difficult to discern brain wave patterns, further delaying a seizure diagnosis and increasing the length of a patient’s stay. Jane Chao, CEO of Ceribell, wants to help fix this. Chao, who has a B.S. in chemistry from Peking University and a Ph.D. in biophysics from Cornell University, has always wanted to work on a problem with a human impact. She spent a year at film school in search of the human connection, before working at McKinsey and then finding her footing in healthcare. Jane Chao [Photo: Ceribell] Chao cofounded Ceribell in 2014 when she learned about the large clinical need for nonconvulsive seizure detection. Ceribell has introduced a portable EEG headset to the market that a nurse or bedside physician can use. It also has an AI that is is trained on a database which has over 800,000 hours of data. In studies, Ceribell’s system has reduced ICU stays by four days, shaved 19 hours off of EEG wait times. In addition, 18% of Ceribell patients have had better outcomes compared to controls. The market is responding to Ceribell’s clinical successes. The company went public in early October, entering the market at $17 a share and closing the day at $25, raising $207.3 million. Fast Company sat down with Chao to understand why seizure detection is such an important problem and how Ceribell can help. How does Ceribell solve the problem? We addressed three big bottlenecks. The first is getting the EEG. Ceribell comes with a disposable headset that doesn’t require an EEG technician to set up. A nurse or resident can set it up in just about five minutes. The second bottleneck we removed is that typically a bedside physician cannot read an EEG. They rely on very specialized neurologists. Most neurologists don’t know how to read an EEG. They tend to be read by epileptologists or neurophysiologists. Reading an EEG is complex and even specialists call it more of an art than a science. We have an AI, a machine-based algorithm, that can detect the result within a few minutes. The third bottleneck we address is that we can provide continuous monitoring. Seizures are very dynamic. A patient can have seizure for 10 to 20 minutes. They can stop seizing and then they can start again. Whenever a patient starts seizing and an episode lasts for more than five minutes, Ceribell will send a beside alert to staff. Without Ceribell, it is close to impossible to have continuous monitoring. We don’t have enough neurologists to have them staring at a screen non-stop to monitor patients. You mentioned reading an EEG is more of an art than a science. How did you train an AI to read them and provide a diagnosis? It was years of investment. We work very closely with epileptologists. In the early days, we had a group of epileptologists working with our data scientists on a daily basis to guide the algorithm. Today we still work very closely with epileptologists. Also, we’re not seeking to replace neurologists—we are trying to make their life easier. There are some who disagree with the AI. We try to work closely with them and continuously improve the algorithm. We also tried to get data from different patient populations to make sure the algorithm performs well in different populations. I’m assuming if you put an EEG in front of different specialists, sometimes they come up with differing diagnoses or answers. How did you train the AI to label EEG results, especially given that non-experts would be reading Ceribell’s EEG? That’s a really insightful question. Studies show if you put the same EEG in front of different neurologists, they reach different conclusions. Also, if you put the same EEG in front of the same neurologist in different contexts, they might read it differently. We had at least three neurologists label our data, and we go with the majority agreement. In a clinical setting, you only have one neurologist looking at the EEG, so you could say our gold standard is actually higher than clinical practice. What kind of concerns do you get about Ceribell replacing jobs for neurologists and EEG technicians? I’m not worried about Ceribell causing job loss. Neurologists do many different things besides read EEGs, and read EEGs for many different things besides seizures. The field is evolving rapidly. We’re providing

Nonconvulsive seizures can kill patients in the ICU. In one study, one-third of such patients died. Yet getting a patient diagnosed with a seizure in the ER or ICU is not easy. It requires an electroencephalogram (EEG), which measures electrical activity in the brain. Getting an EEG can take anywhere between a few hours to a couple of days, since there is a shortage of EEG technicians. Post-pandemic, one study reported that EEGs have declined by 50%.
If a doctor decides to treat a patient proactively without a diagnosis, treatment can be invasive and might mean being intubated and being dosed with benzodiazepines. Taking benzodiazepines prior to an EEG makes it difficult to discern brain wave patterns, further delaying a seizure diagnosis and increasing the length of a patient’s stay.
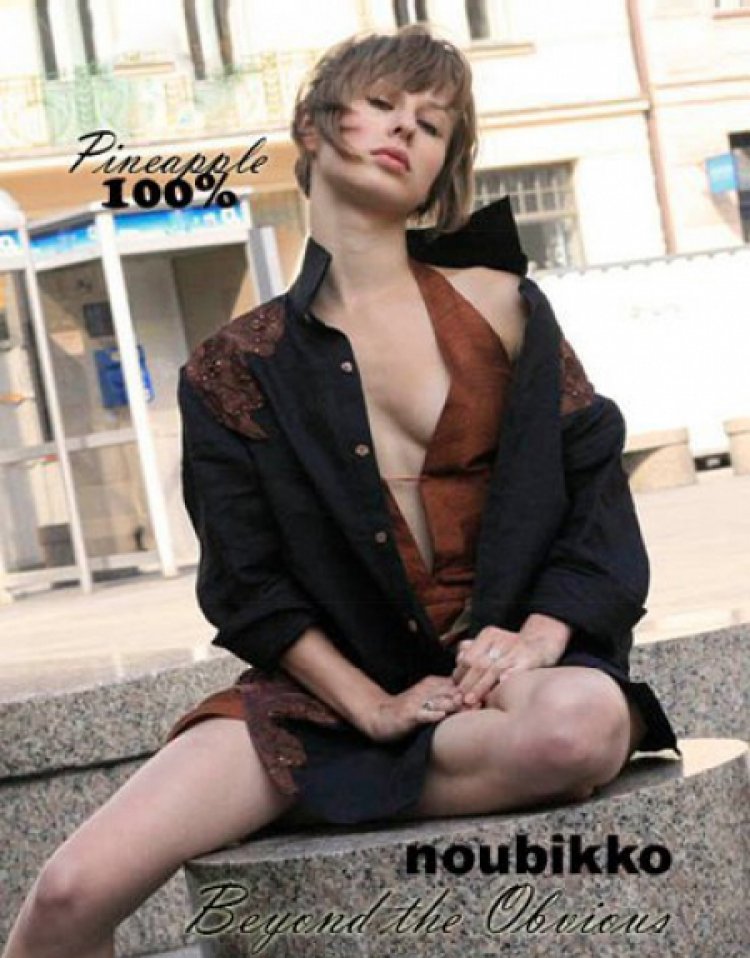
Jane Chao, CEO of Ceribell, wants to help fix this. Chao, who has a B.S. in chemistry from Peking University and a Ph.D. in biophysics from Cornell University, has always wanted to work on a problem with a human impact. She spent a year at film school in search of the human connection, before working at McKinsey and then finding her footing in healthcare.

Chao cofounded Ceribell in 2014 when she learned about the large clinical need for nonconvulsive seizure detection. Ceribell has introduced a portable EEG headset to the market that a nurse or bedside physician can use. It also has an AI that is is trained on a database which has over 800,000 hours of data. In studies, Ceribell’s system has reduced ICU stays by four days, shaved 19 hours off of EEG wait times. In addition, 18% of Ceribell patients have had better outcomes compared to controls.
The market is responding to Ceribell’s clinical successes. The company went public in early October, entering the market at $17 a share and closing the day at $25, raising $207.3 million.
Fast Company sat down with Chao to understand why seizure detection is such an important problem and how Ceribell can help.
How does Ceribell solve the problem?
We addressed three big bottlenecks. The first is getting the EEG. Ceribell comes with a disposable headset that doesn’t require an EEG technician to set up. A nurse or resident can set it up in just about five minutes.
The second bottleneck we removed is that typically a bedside physician cannot read an EEG. They rely on very specialized neurologists. Most neurologists don’t know how to read an EEG. They tend to be read by epileptologists or neurophysiologists. Reading an EEG is complex and even specialists call it more of an art than a science. We have an AI, a machine-based algorithm, that can detect the result within a few minutes.
The third bottleneck we address is that we can provide continuous monitoring. Seizures are very dynamic. A patient can have seizure for 10 to 20 minutes. They can stop seizing and then they can start again. Whenever a patient starts seizing and an episode lasts for more than five minutes, Ceribell will send a beside alert to staff. Without Ceribell, it is close to impossible to have continuous monitoring. We don’t have enough neurologists to have them staring at a screen non-stop to monitor patients.
You mentioned reading an EEG is more of an art than a science. How did you train an AI to read them and provide a diagnosis?
It was years of investment. We work very closely with epileptologists. In the early days, we had a group of epileptologists working with our data scientists on a daily basis to guide the algorithm. Today we still work very closely with epileptologists.
Also, we’re not seeking to replace neurologists—we are trying to make their life easier. There are some who disagree with the AI. We try to work closely with them and continuously improve the algorithm.
We also tried to get data from different patient populations to make sure the algorithm performs well in different populations.
I’m assuming if you put an EEG in front of different specialists, sometimes they come up with differing diagnoses or answers. How did you train the AI to label EEG results, especially given that non-experts would be reading Ceribell’s EEG?
That’s a really insightful question. Studies show if you put the same EEG in front of different neurologists, they reach different conclusions. Also, if you put the same EEG in front of the same neurologist in different contexts, they might read it differently. We had at least three neurologists label our data, and we go with the majority agreement. In a clinical setting, you only have one neurologist looking at the EEG, so you could say our gold standard is actually higher than clinical practice.
What kind of concerns do you get about Ceribell replacing jobs for neurologists and EEG technicians?
I’m not worried about Ceribell causing job loss. Neurologists do many different things besides read EEGs, and read EEGs for many different things besides seizures. The field is evolving rapidly. We’re providing a tool to make their life easier.
In the case of EEG technicians, first we focus on ICU and emergency departments, not outpatient settings, where most EEG technicians work. We have no plans to go into the outpatient settings.
There’s a huge national shortage of EEG technicians. Many of them have back-to-back scheduled EEGs for outpatient settings, and when they are called to the ICU they have to drop everything, run to the ICU, set up the urgent EEG, and run back to the outpatient clinic. It’s very stressful. If they get a night call, they have to come in at night and then work again the next day. We’re helping EEG technicians take care of more patients in a more efficient and effective way.
What’s on the horizon?
We want to become the standard of care for seizure management in the acute care settings such as the ICU and the emergency department. Our north star is really no patient should suffer brain injury or even potential deaths because of a delayed EEG.
The second horizon is to make an EEG a new vital sign. The brain actually still remains a black box. We monitor so many organs, but we barely monitor our brains. We started the company because we saw there’s a big patient unmet need and we wanted to provide the right tools to solve it.